
Even though the content will go Live, different resources will be made available on the app/website as they are built/updated.
The content will be subject to the following provisos:
- The content will be subject to continuous update and review
- Old content (from previous CGOs) will be converted into the new format, using new tools
- Content will be moved around
- The layout will change and reflect the needs of the user
- Content will be created
- Content will be deleted/retired
CGO development will continue.
Saf
[Updated 2 Apr 2024]
Content coming soon...
Content coming soon...
Content coming soon...
Content coming soon...
Content coming soon...
Content coming soon...

Features (may be delayed)
• Chest pain
• Hyperinflated hemithorax
• Splayed ribs
• Extreme respiratory distress (consistent; refractory to reassurance)
• Low SpO2
• Reduced/absent breath sounds
• Hyperresonance
• Reduced/absent movement on affected side
• Late signs: hypotension; trachea deviated away from affected side;
distended neck/ chest/upper arm veins (inconsistent sign if hypovolaemia)
Needle decompression (affected side)
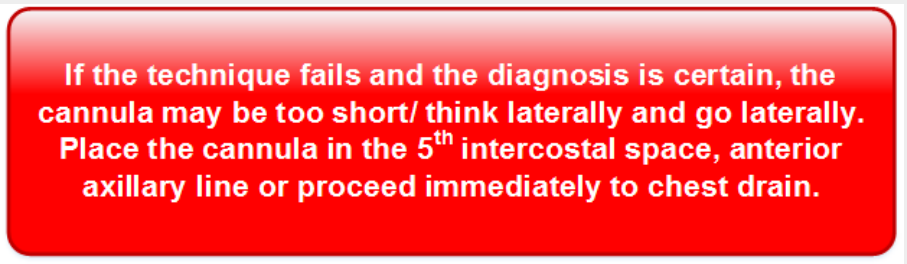
Locate second intercostal space mid-clavicular line on affected side (2nd rib joins the
sternum at the sternal angle; 2nd intercostal space is below this rib).
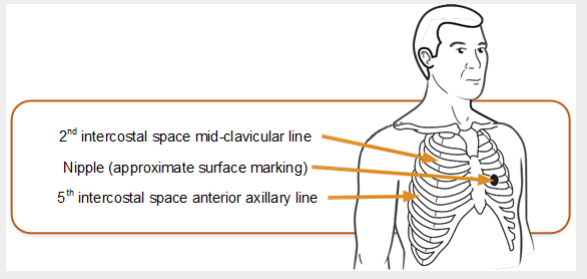
• Insert the needle decompression device perpendicularly into the chest, just above the
3rd rib. Air may be heard escaping.
• Secure the device in place and check the patient for signs of improvement.
• Document the procedure (this is important if the device is removed/falls out before the
casualty reaches hospital)
Definitive care
• A chest drain is required
Features (immediate)
• Low SpO2
• Hypotension
• Surgical emphysema
• High inflation pressures
• Affected side showing over-expansion (ribs splayed), reduced mobility,
reduced/absent breath sounds, increased resonance
• Late signs: trachea deviated away from affected side
• Distended neck/chest/upper arm veins (inconsistent sign if hypovolaemia)
• Potential for bilateral tension pneumothorax
Needle decompression (affected side)
Locate second intercostal space mid-clavicular line on affected side (2nd rib joins the
sternum at the sternal angle; 2nd intercostal space is below this rib).
Definitive Care
• A chest drain is required
Features
• Shock (tachycardia and hypotension)
• Affected side showing: reduced breath sounds, dullness to percussion,
under-expansion and reduced mobility
• Respiratory distress (mild – severe)
If a massive haemothorax is present, gain IV access, consider giving blood products and
TXA.
Give analgesia and antibiotics in line with DMS Deployed Antibiotic Policy
For Haemorrhagic shock:
Go to
Myocardial Infarction and Acute Coronary Syndromes ( link to NICE guideance)
Evacuate to definitive care as T1
Features
• Low SpO2
• Respiratory distress
• “Sucking” and bubbling from the wound
• Shock
• Affected side showing reduced movement, absent breath sounds, reduced
mobility (under-expansion), increased resonance
First aid
• Apply Russell Chest Seal and reassess.
• A chest drain may be required if there is a prolonged hold and an
appropriate skill set available.
• Ventilate if there is respiratory compromise despite presence of chest
drain.
For haemorrhagic shock go to:
Go to
Myocardial Infarction and Acute Coronary Syndromes ( link to NICE guideance)
Evacuate to definitive care as T1
Features
• Severe chest pain
• Extreme respiratory distress
• External signs of blunt chest injury (bruising/swelling/seatbelt marks)
• Crepitus: fractured ribs/surgical emphysema
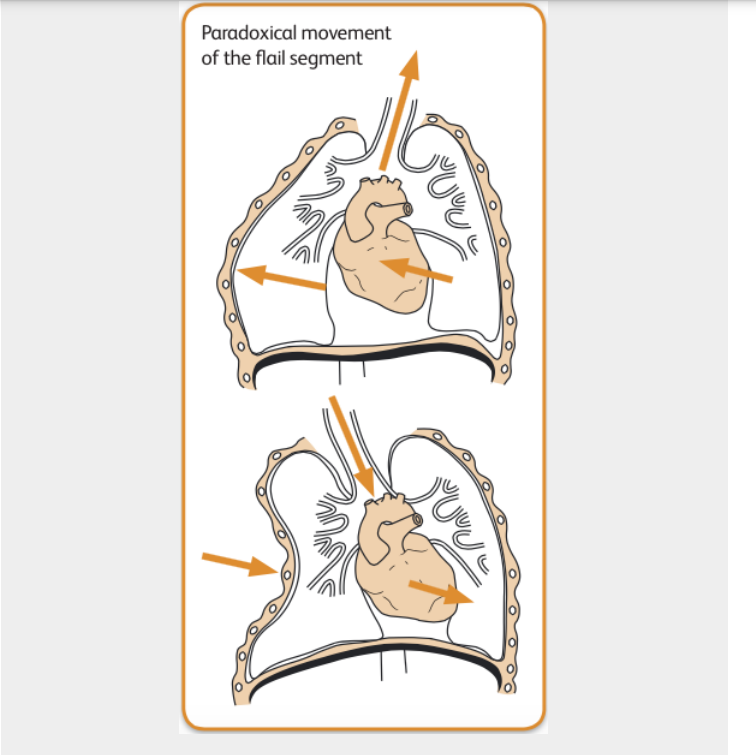
• Paradoxical movement of the flail segment (see diagram, may be subtle),
or hypomobility
• Low SpO2
• Signs from associated haemothorax may be present
Resuscitation
• Critical decision: exclude or treat associated tension (key indicator is overinflation
of hemithorax). Remember that needle decompression in absence of tension
might make the patient’s condition worse.
• A chest drain (technically may be difficult) will be needed for failed
decompression, large simple pneumothorax. There is a low threshold for postventilation chest drain because of the risk of tension pneumothorax.
• Continuing treatment is principally directed towards the underlying contusion.
Where there is respiratory compromise (hypoxia and/or hypercapnia) on blood
gases proceed to ventilation (Rapid Sequence Induction of anaesthesia by
trained staff only).
Go to: Airway Compromise
First aid
• Evacuate T1 with affected side down (will offer some splinting of segment).
BATLS resuscitation
• Critical decision: exclude or treat associated tension (key indicator is overinflation
of hemithorax). Remember that needle decompression in absence of tension
might make the patient’s condition worse.
Features
• An injury where there is initially diffuse bleeding with the lung (causing
hypoxia), which progresses to an inflammatory state with the lung.
• Blast Lung Hypoxia can get rapidly worse: or develop over 24-48 hours.
• Small number of these patients present with severe refractory hypoxia very
soon after injury
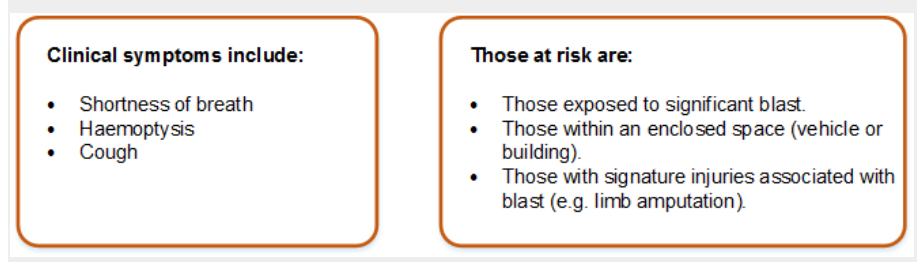
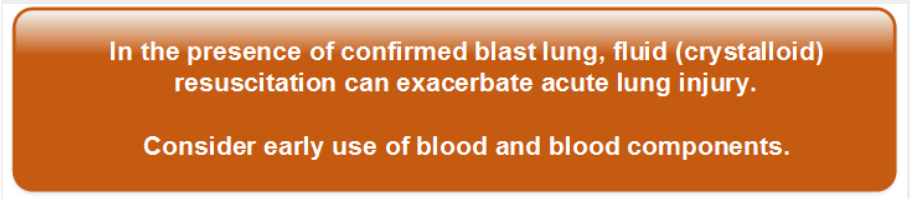
Guidance for Management • Initial resuscitation follows standard DMS ABC protocol. − Give high flow oxygen to maintain SaO2 over 95%. • Actively exclude pneumothorax and haemothorax.
Features
• Pneumothorax may occur spontaneously in the absence of trauma.
• Pneumothorax may also be secondary to asthma, pneumonia or TB.
• Sudden onset unilateral pleuritic chest pain
• Dyspnoea +/– cough.
• Depending on size of pneumothorax there may be tachypnoea and
tachycardia and percussion may be normal or hyperresonant.
Investigations
• CXR is essential to diagnose small pneumothoraces: the stethoscope is only a
crude diagnostic aid.
• Monitor SpO2.
• Measure ABG when there is dyspnoea and/or reduced SpO2.
• ECG when the prominent symptom is chest pain.
Treatment
• Aspiration is recommended for spontaneous pneumothorax:
– infiltrate with local anaesthetic, insert a 16G IV cannula in the 2nd intercostal
space
in the mid clavicular line
– attach three way tap and aspirate with a 50ml syringe
– continue aspiration until patient coughs excessively or until 2.5 litres of air is
removed.
• If aspiration unsuccessful insert a chest drain.
Where no chest X-ray capability is available, the patient is symptomatic
and clinically there is a pneumothorax, insert a chest drain
Note
Ultrasound can be used successfully to detect a pneumothorax.





Venous thromboembolic (VTE) disease (deep vein thrombosis, DVT, +/–
pulmonary embolic disease, PED), is a major contributor to morbidity and
mortality in hospital admissions across all specialities. Studies have shown
that 0.9% of all hospital admissions will die of PED, 10% of all hospital deaths
are due to PED and the risk of VTE rises tenfold in patients hospitalised after
trauma, surgery or immobilising medical illness.
• VTE thromboprophylaxis is to be given unless there is a clear indication to the
contrary. The decision NOT to give prophylaxis should be made by a senior
clinician and reasons for this decision recorded in the clinical notes.


Notes
• Below-knee GECS are NOT to be used
• LMWH does not require coagulation monitoring
• Aspirin not suitable for prophylaxis as of unproven efficacy
• Duration of therapy is until fully mobile or discharge from hospital